Does Obesity Literally Accelerate Aging?
It is well known that carrying excess visceral fat tissue increases risk of age-related disease, shortens life expectancy, and raises lifetime medical expenditure. The more fat tissue, the worse the outcome, but even being modestly overweight rather than obese still produces a negative impact on long term health. This is the story told in a great many epidemiological studies with large patient populations. Does this mean that obesity accelerates aging, however? It might be surprising to find out that this isn't a question that has an easy or a straightforward answer.
In order to talk about whether aging is accelerated, one has to have a strong understanding of what causes aging. If we can list specific causative mechanisms of aging, and then measure their state, then we might be able to say whether or not aging is accelerated or slowed by a given circumstance. In the SENS view of aging, the root cause is accumulation of cell and tissue damage that arises as a side-effect of the normal operation of cellular metabolism. Things like the presence of lingering senescent cells or cross-links in the extracellular matrix. We can make the argument that a lifestyle choice that increases the pace at which senescent cells emerge in tissues is in fact an acceleration of aging. We can similarly argue that environmental circumstances such as smoking or chemotherapy that do the same have some component of accelerated aging in the harm that they cause.
Excess visceral fat tissue does in fact add to the presence of senescent cells. It also causes chronic inflammation via several other mechanisms, distinct from that of the inflammatory signaling produced by senescent cells. The chronic inflammation of aging is a downstream consequence of causes of aging, but it is a prominent feature of aging and causes further issues in and of itself, speeding up the progression of all of the common age-related conditions. Could upregulating inflammation directly, without going via one of the underlying causes of aging, be called an acceleration of aging? Perhaps not. Perhaps it should just be called harm and damage, and fall into the same category as breaking a bone and the long-term consequences that result from that sort of injury. So we might say that fat tissue accelerates aging in some senses, but in others it is not an acceleration of aging, just a harm.
This may be a matter of semantics and definitional games. The lesson at the end of the day is to avoid putting on excess weight, as even therapies targeting the causes of aging cannot prevent all of the long-term damage that being overweight will generate. Different perspectives are always interesting, however. Today's open access paper, noted below, looks at the question of whether or not obesity accelerates aging through the filter of the Hallmarks of Aging, a more recent catalog of potential causes and mechanisms of aging that overlaps to some degree with the causes of aging listed in the SENS proposals, but has significant differences. Some of the Hallmarks are clearly downstream consequences or markers of the progression of aging from the SENS perspective, for example.
Obesity May Accelerate the Aging Process
It has been suggested that obesity not only increases the onset of metabolic imbalances, but also decreases life span and impacts cellular processes in a manner similar to aging. A defining characteristic of aging is the gradual loss of physiological integrity, which results in increased vulnerability to disease and death. This loss of physiological integrity underlies multiple pathologies, including cancer, diabetes, cardiovascular disorders, and neurodegenerative disease. Recently, nine hallmarks which define the aging process have been described. We will briefly discuss each of the hallmarks of aging and the potential interactions between each hallmark and obesity.
Based on the evidence, two distinct hypotheses can be proposed. One is that the cellular responses provoked by an excess of nutrients cause obesity, and that obesity is responsible for accelerating the pace of aging. Supporting this hypothesis are the observations that knocking out the fat-specific insulin receptor, to produce extremely lean mice, and removal of visceral fat in rats increased life span; additionally, calorie restriction on lean strains of rats, had only a minor effects on lifespan. The alternative possibility is that the cellular responses provoked by an excess of nutrients are responsible for increasing the pace of aging. This common soil shared by both aging and obesity has been named "adipaging", and there is some evidence of commonalities: hyperglycaemia, for example, induces senescence and the SASP in endothelial cells and macrophages while glucose reduction prevents replicative senescence in human mesenchymal stem cells.
Telomere Attribution
Obesity causes oxidative stress and inflammation, which may increase the rate of telomere shortening. Although the association is weak or moderate, results show a trend toward a negative association between obesity, in particular central obesity, and telomere length. Human studies indicate that telomere shortening is directly correlated to adiposity, and telomere length is inversely associated with BMI. However, this association is not linear across the age and it is stronger in younger compared to older individuals. We feel that although the results cumulatively show a tendency toward an inverse correlation between obesity and telomere length; it is more prudent to conclude that the available studies are heterogeneous and show a weak statistical significance.
Epigenetic Alteration
Several studies demonstrated that obesity is associated with extensive changes in gene expression in multiple tissues and that increased BMI is associated with an altered methylation of specific genes. For instance, it was shown that obesity is associated with methylation changes in blood leukocyte DNA that could lead to immune dysfunction. Investigation of the association between BMI and epigenetic age in blood cells demonstrated that BMI is positively associated with epigenetic aging in middle-aged individuals. The impact of obesity on epigenetic aging is also described: obesity accelerates epigenetic changes associated with aging in the human liver resulting in an apparent age acceleration of 2.7 years for a 10-point increase in BMI, supporting the idea that obesity may accelerate the aging process.
Mitochondrial Dysfunction
Obesity has also been associated with mitochondrial dysfunction. Calorie restriction, conversely, which increases longevity, maintains mitochondrial function. Several studies showed that obesity induces a reduction in mitochondrial biogenesis and a decreased mitochondrial oxidative capacity in adipocytes of both rodents and humans. In obese individuals, reduced mitochondrial biogenesis is associated with metabolic alterations, low-grade inflammation, and insulin resistance. Several lines of evidence suggest that obesity induces a shift toward a fission process linked to mitochondrial dysfunction in liver and skeletal muscle. In skeletal muscle of obese mice, an increased mitochondrial fission was observed and the activity of protein involved in mitochondrial dynamic was altered. Aging and obesity appear superimposable in their impact on mitochondria and it is reasonable to hypothesize that they could exert additive effects.
Cellular Senescence
It has been demonstrated that SA β-gal+ cells are more abundant in pre-adipocyte and endothelial cells isolated from obese compared to lean rats and human, moreover there is a positive correlation between BMI and adipose tissue SA β-gal activity and p53. There is an accumulation of senescent T cells and an increased number of macrophages in the inflammatory foci of the visceral adipose tissue of obese mice, and obese mice accumulate senescent glial cells in the brain. There appears to be a strong relationship between obesity and senescence. Obesity may promote the aging process by inducing senescence. Conversely, senescence and the resulting pro-inflammatory secretory phenotype could contribute to the morbidity associated with obesity and plays a role in the development of insulin resistance and diabetes. There is a vast literature in support of this view.
Deregulated Nutrient Sensing
In biogerontology, the IIS and mTOR pathway are considered "accelerators" of the aging process. There is accumulating literature suggesting that in obesity, these pathways are over-activated. In contrast, there is also accumulating literature showing that pro longevity pathways, such as the AMPK and sirtuins pathways are dampened by obesity. In conclusion, there is solid evidence that obesity deregulates cellular mechanisms related to nutrient sensing.
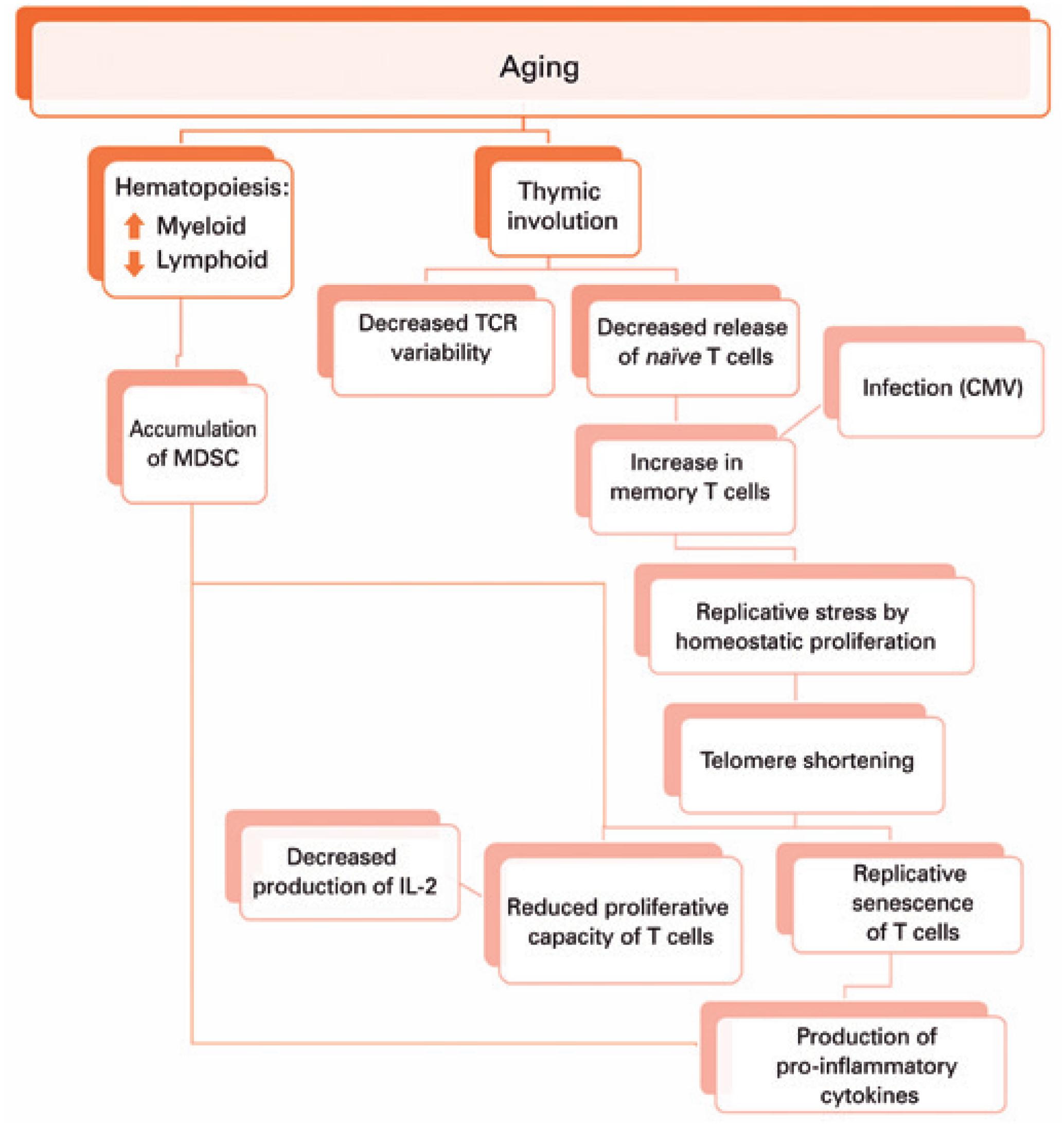
Altered Intercellular Communication
It is accepted that aging impacts the organism at the cellular level, but also decreases the capacity of cells of an organism to interact. During aging, there is a decreased communication at the neuronal, neuroendocrine, and endocrine levels. Two of the most compelling examples of impaired communication are inflammaging and immunosenescence. The inflammaging phenotype results in elevated cytokines. These cytokines can accelerate and propagate the aging process. The literature persuasively suggests that the accumulation of pro-inflammatory cells, in the adipose tissue of obese patients, through cytokines and extracellular vesicles, accelerates the rate of aging both in the adipose tissue itself and the entire organism.
Genomic Instability
The impact of obesity on genomic instability has been analyzed. Results from animal studies and studies in humans, monitoring DNA damage in lymphocytes and sperm, were analyzed. However, heterogeneity in the study design, methodology, and confounding factors, preclude the conclusion that an association exists between obesity and DNA damage. Nevertheless, the causal relation between excess of body weight and genomic instability is supported by mechanistic studies. Oxidative damage seems as the one mechanism regarded as the most relevant.
Loss Of Proteostasis
With age, the ability of many cells and organs to preserve proteostasis under resting and stressful conditions is gradually compromised. Key pathways affected by the aging process alter components of the proteostasis machinery, e.g., by inducing reduction of chaperones or proteasomal degradation. Obesity can induce prolonged or chronic unfolded protein response possibly mediated by proteasome dysfunctions. In the livers of mouse models of obesity, proteasome activity is reduced and polyubiquinated proteins accumulate. In these mice, impaired proteasome function leads to hepatic steatosis, hepatic insulin resistance, and unfolded protein response activation. Treatment with chemical chaperones partially reverted this phenotype.